O/E : large 15 x 12 cm mass palpable arising from liver left lobe, hard, nontender.
NO Anorexia, No wt loss.
AFP, CEA,CA 19.9, CA 125 Were normal
CT / MR Abdomen angio:
s/o malignant liver mass from segment 3, hanging in nature with doubtful lesion in seg 4b as well.
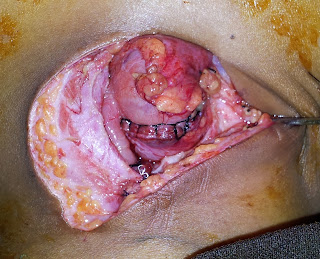
SURGERY: Left hepatectomy with excision of seg 4b lesion, DURATION: 4.5 hrs. No blood transfusion required..and pt was shifted to ward post operatively..
was discharged on POD 5, With normal diet, and without any undue complication..
HPE : IHC S/o Hepatoblastoma, node negative, resection margins free of tumor..
pt subjected to adjuvent chemotherapy to totally eradicate the disease..
www.gisurgerysurat.com
www.sidshospital.com
You Tube : Dr Keyur Bhatt
Dr. Keyur Bhatt - Best
Gastro Surgeon
Dr. Keyur Bhatt- Best GI
Surgeon
Dr. Keyur Bhatt - Best
Gastro Surgeon
Dr. Keyur Bhatt- Best GI
Surgeon - Dr Keyur Bhatt - Best Gastro Surgeon
Dr. Keyur Bhatt- Best GI
Surgeon - Dr Keyur Bhatt - Best Gastro Surgeon
Dr Keyur
Bhatt- Best GI Surgeon