found to have ? CBD Stone. ERC and cleared & stented
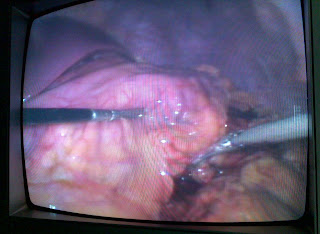
post procedure pancreatitis ...kept conservatively ...improved..but unfortunately developed gangrenous cholecystis with perforation.
SURGERY: OPEN chelecystectomy
post op biliary fistula sattleing down conservatively...
www.gisurgerysurat.com
www.sidshospital.com
You Tube : Dr Keyur Bhatt
Dr. Keyur Bhatt - Best
Gastro Surgeon
Dr. Keyur Bhatt- Best GI
Surgeon
Dr. Keyur Bhatt - Best
Gastro Surgeon
Dr. Keyur Bhatt- Best GI
Surgeon - Dr Keyur Bhatt - Best Gastro Surgeon
Dr. Keyur Bhatt- Best GI
Surgeon - Dr Keyur Bhatt - Best Gastro Surgeon
Dr Keyur
Bhatt- Best GI Surgeon